The joints of the human body resist daily stress, making them susceptible to various types of destructive factors. Among joint diseases, osteoarthritis is common and affects both large and small joints. Arthrosis of the knee joint is a degenerative-dystrophic damage to the knee joint, in which its motor activity is impaired. In the absence of proper treatment, the disease can lead to disability.
As the disease causes characteristic deformities in the joint, it was called deforming arthrosis of the knee joint, which correctly describes the typical feature of the pathology. The disease is chronic and most often diagnosed in women, in addition, those who suffer from overweight and venous pathologies of the lower extremities, but there may be other reasons. Due to age-related changes, it also occurs in older people.
Osteoarthritis in young people can be triggered by injuries. As a result of degenerative-dystrophic changes, the cartilage softens, exfoliates and becomes covered in cracks of various depths. Subsequently, it ceases to perform its function.
The reasons
Several causes lead to the appearance of deforming arthrosis of the knee joint. The traumatic factor is a common cause of occurrence. Post-traumatic osteoarthritis can develop as a result of a dislocation or fracture in the specified area, as well as a meniscus tear. Usually, knee joint gonarthrosis appears in young people who are actively involved in sports or in those people whose work is associated with increased mobility, lifting and carrying heavy loads.
Few people know that this damage can also be a result of treatment, when the injury itself has already healed, but during prolonged immobilization of the limb, circulatory disorders occurred in this area. Because of this, gonarthrosis appeared.
The increase in physical activity in the knee is one of the main factors in the onset of the disease. It most often affects athletes who have constant active loads on the knee. At a young age, osteoarthritis may not manifest itself, usually rapid changes begin after the cessation of physical activity.
There is also a risk of disease in those people who, even in adulthood, do not reduce the load on the joints. In these athletes, the risk of fractures and dislocations increases, microtraumas appear. Therefore, already after forty years, doctors recommend that athletes reduce the load, switch to training. Running and squats should be avoided as these are the activities that put the most strain on the knee joint. Most often, one limb is affected and left-sided gonarthrosis or right-sided gonarthrosis occurs.
An essential factor for the development of osteoarthritis of the knee joint is the removal of the menisci. If for some reason the menisci were removed, in 90% of cases this leads to the appearance of arthrosis - the so-called looping of the knee occurs, during which the joint joints experience more friction than normal.
The problem of being overweight is also relevant for people with osteoarthritis. Excess body weight puts unnecessary strain on joints. As a result, not the cartilage itself is damaged, but the meniscus. And with a combination of overweight and varicose veins of the lower extremities, acute arthrosis threatens to appear.
Weak ligament apparatus in some patients is a congenital feature and sometimes the ligaments are affected due to other diseases. One way or another, weak ligaments cause increased mobility in the joint, due to which the joint surfaces are significantly worn down. The consequences of weak ligaments may not be felt for a long time until patients show symptoms of true osteoarthritis.
Joint pathologies also lead to the development of the disease. The most common cause of osteoarthritis is arthritis - inflammation of the joint joints. With arthritis, typical signs are observed - deterioration in the composition of synovial fluid, pathological changes in cartilage, swelling, redness of soft tissues. Even after osteoarthritis is cured, chronic processes lead to the appearance of osteoarthritis.
Violations of metabolic processes often lead to pathologies of the musculoskeletal system. Bones and joints lack the nutrients and minerals that are so necessary for tissue strength. With their lack, bones and cartilaginous surfaces are subject to destructive processes, therefore, even with a light load, primary arthrosis arises.
Symptoms
Osteoarthritis of the knee joint is manifested by a complex of characteristics that are difficult to miss. The signs are not only felt in the first stage of development of the pathology, but the second and third stages give different symptoms of arthrosis of the knee joint:
- pain- one of the main signs that does not appear immediately. An interesting fact is that with the development of osteoarthritis, pain may not be felt for several months or years, until the disease worsens. Usually, the first signs of pain are discomfort during physical exertion, walking or running, but it also manifests when the meniscus is compressed. With the second degree of osteoarthritis, pain in the joint is felt more strongly, and with the third degree of development, painful sensations appear even at rest. Attacks are aggravated even after short walks without a heavy load on the joint, so patients try to spare their knees;
- deformations- the manifestations become more pronounced in the third stage of the development of arthrosis. The knee will retain its normal shape but will appear slightly swollen and oedematous. When arthritis sets in, the knee becomes red, hot and painful to the touch;
- crushwith arthrosis appears in the second and third stage of development of the disease. The crunchy sounds are different from the healthy clicks that can sometimes be heard when the knee is extended and flexed. In osteoarthritis, symptoms are characterized by a dry, harsh sound that comes on abruptly and is accompanied by pain;
- synovitis- accumulation of a certain amount of fluid in the joint cavity. It's there and it's normal. But the accumulation of an excessive amount leads to the development of a cyst - the most noticeable Baker's cyst, which can be determined in the unbent position of the leg;
- limited knee mobility- a typical sign of pathology, as patients first consciously try to protect themselves from pain, and in the final stage of arthrosis, they are unable to straighten the limb. In the third stage of development, deforming osteoarthritis of the knee joint (DOA) completely leads to loss of movement. Patients adapt to move with their legs bent while using the means of support.
degrees of development
Osteoarthritis of the knee joint goes through three stages in its development.
With 1st degree osteoarthritis, pain is negligible and occurs only with active physical exertion on the knee joint. Already in the first degree, fluid can accumulate in the cavity, which in the second and third is already a cyst. With progression, pain occurs during movement but passes quickly. Externally, the deformation of the knee joint is invisible, so the diagnosis of osteoarthritis of the knee joint can be difficult.

With a second-degree disease, damage to cartilage tissue is more significant. If you take an x-ray, the bone growth stage is already noticeable. With any movement, a sudden sharp pain appears in the knee, but, returning to a comfortable position, the knee no longer hurts. In the second stage of DOA, you can hear a crunch typical of osteoarthritis. With progression, knee extension and flexion problems worsen. The deformation becomes externally noticeable.
Third degree osteoarthritis of the knee joint is characterized by significant thinning of cartilage tissue. Gradually, the cartilage wears out so much that the bone is exposed in some areas. An x-ray image shows a significant amount of osteophytes - bone growths, salts that have appeared in the joint cavity. Externally, the changes are clearly visible and the patient is worried about constant pain. It is not difficult to make a diagnosis - a visual examination is sufficient and X-ray control is carried out.
With the progression of this degree, osteoarthritis can lead to a complete loss of functionality. At any stage of development of the pathology, osteoarthritis of the knee joint can join.
Treatment
Dealing with osteoarthritis of the knee joint is not easy, especially if the disease is advanced or inflammation has joined and arthritis has developed.
conservative
The group of the most active drugs against osteoarthritis are non-steroidal anti-inflammatory drugs. These are mainly cyclooxygenase-2 inhibitors, they can perfectly relieve inflammation, swelling and contribute to speedy recovery.
These medications have significant limitations, so they should not be used without a doctor's recommendation. For example, they are able to exacerbate stomach ulcers, heart disease, pathology of Organs urinary organs. Non-steroidal anti-inflammatory drugs are also prohibited during pregnancy.
The second group of agents are the chondroprotectors that improve the characteristics of cartilage tissue. They are used for osteoarthritis to restore the correct structure of cartilage, because in the process of resolution it loses very important components - chondroitin and glucosamine. Therefore, almost all chondroprotectors contain these two substances, but some preparations are monocomponents.
With the help of these drugs, it is possible to help the patient in the first and second stages of the development of the disease, but not in the third, when irreversible changes occur.
During conservative therapy, the doctor will also give recommendations on nutrition. If the patient or patient is overweight, it is imperative to follow a diet to normalize the weight. How to strengthen a stable weight - the doctor will also tell. It is also not recommended to eat a lot of salt, but it is better to fill the diet with calcium, vitamins and minerals. Jelly, jelly will be useful.
operational
The most common type of surgery for osteoarthritis is arthroscopy, but other interventions are performed. Treatment of osteoarthritis of the knee joint is usually carried out in the second and third degree, when conservative therapy no longer helps.
If minimally invasive intervention is required, for example when fluid accumulates in the knee joint, a puncture can be performed. A puncture is made in the cavity of the knee joint and excess fluid is pumped out. This method can diagnose a disease and simultaneously apply it to treatment. Liquid is taken at the initial stage in a minimal amount, but this already significantly improves the well-being of patients. Then, after examining the biomaterial, another part is removed and corticosteroids are injected into the joint cavity.

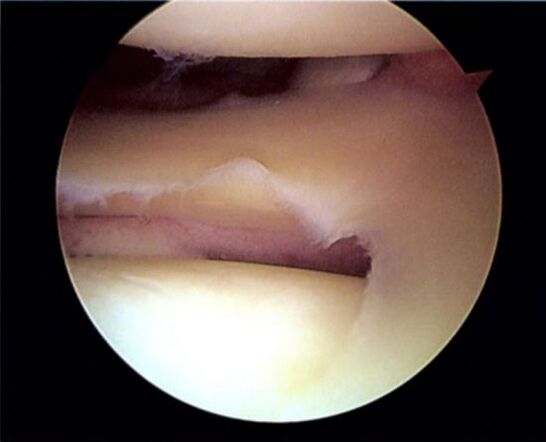
Arthroscopy is the most common. Through a small incision in the skin, several instruments are introduced that allow the examination of the joint and the necessary manipulations in it. With the help of arthroscopy, it is possible to remove tissue particles that have separated from the cartilage, but there is always a risk of secondary gonarthrosis.
With severe damage, there is a need to perform a periarticular osteotomy. This is a larger scale impact on the joint, as a result of which it is filed a little and adjusted to the desired angle. After the operation, rehabilitation takes longer, but the effect lasts longer.
Significant destruction of joint elements leads to complete immobilization of the limb. The gasket does not fulfill its function, which means it needs to be replaced and an operation needs to be done. Knee joint endoprosthesis is an expensive operation, but in itself it allows the patient to return to limb movement. Various knee prostheses are installed - plastic, ceramic or metal. They are durable structures that allow you to forget about the problem for several decades.
Physiotherapy
Physiotherapy methods can only be used when the acute period has passed and the patient is recovering.
Actively used methods include:
- ozone therapy- exposure of the affected joint to ozone, which can be injected or used as an external treatment. This type of patient care is very effective, so it is often used in the treatment of various pathologies, including arthrosis. The treatment allows to activate blood circulation in the problem area, to obtain an anti-inflammatory and analgesic effect. At the same time, treatment with glucocorticoids is carried out;
- kinesiotherapy- treatment is carried out with the help of a special set of exercises. The load is formed taking into account individual data, and when performing exercises, special simulators are used that strengthen the joints. The difference between kinesiotherapy and physical therapy exercises is the active effect not only on knee osteoarthritis, but also on the whole body as a whole.
Apply not only ozone therapy and kinesiotherapy, but also physical therapy. Good results are given by the author's exercise methods to eliminate knee arthrosis. During and after the exercises, you may need to wear a special knee brace - an orthosis, to strengthen the right or left knee joint.


















